A herniated disc can cause anything from mild discomfort to severe pain that radiates down your leg. The good news is that most cases improve without surgery. Understanding your condition is the first step toward recovery, and this guide will help you make informed decisions about your care.
What Is a Herniated Disc?
A herniated disc occurs when the soft, gel-like center of a spinal disc pushes through a tear in the tougher outer layer, potentially pressing on nearby nerves and causing pain that radiates down the leg or arm depending on which disc is affected.
Your spine consists of 24 vertebrae stacked on top of each other. Between each pair of vertebrae sits a disc that acts as a shock absorber and allows your spine to move. Think of each disc like a cushion: the outer layer (annulus fibrosus) is tough and rubbery, while the inner core (nucleus pulposus) is soft and gel-like.
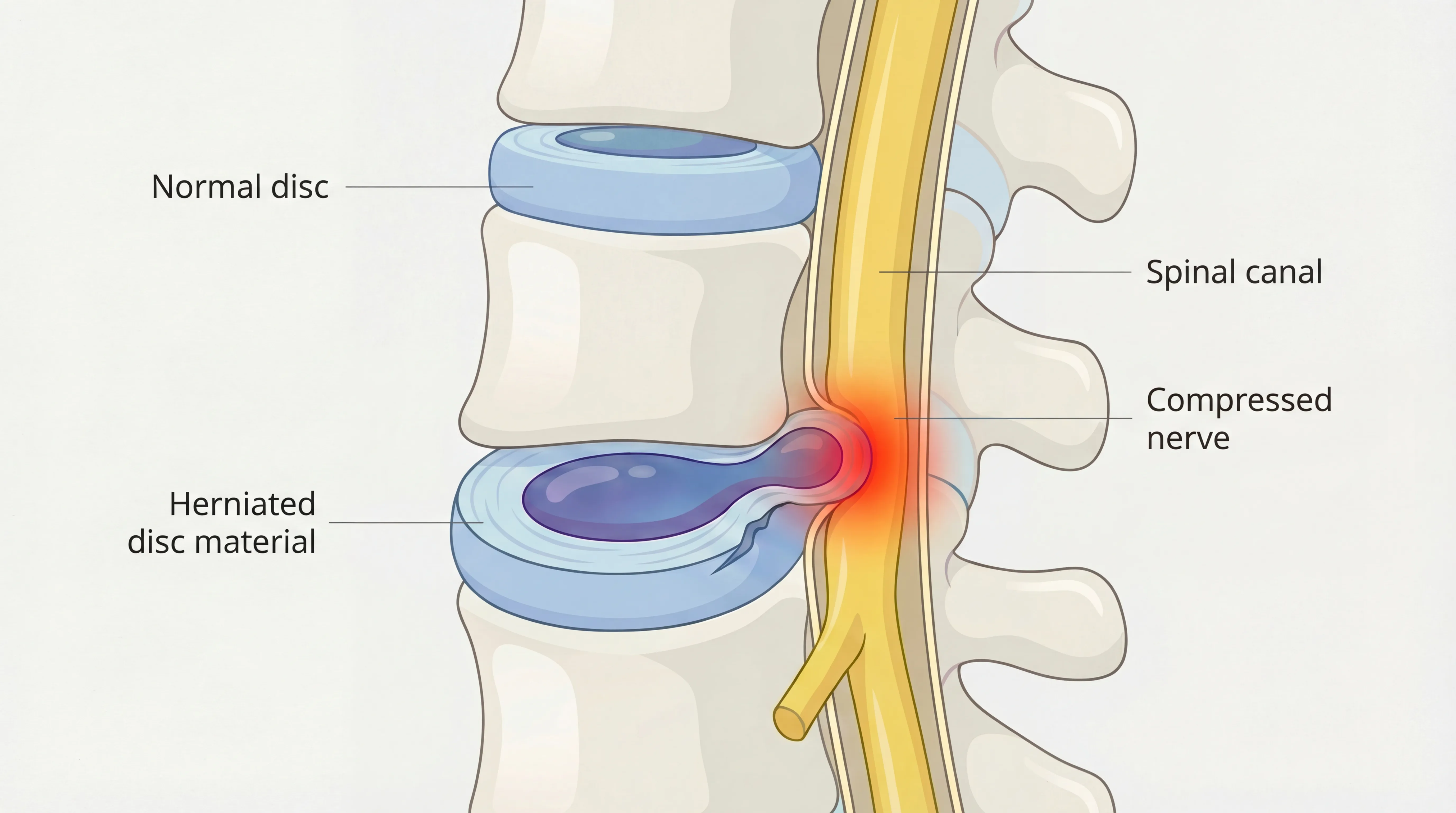
When the outer layer develops a tear, the inner material can push outward. This is called herniation. The herniated portion may press against spinal nerves, causing pain that can travel down your arm or leg depending on which disc is affected.
Common locations
Herniated discs most often occur in two areas:
- Lumbar spine (lower back): L4-L5 and L5-S1 are the most common locations, causing pain that often radiates down the leg
- Cervical spine (neck): C5-C6 and C6-C7 are typical sites, causing pain or numbness that travels down the arm
Thoracic herniations (mid-back) are rare because this part of the spine doesn't move as much.
Herniated vs. bulging vs. degenerative
These terms describe different disc conditions:
- Bulging disc: The disc extends outward but the outer layer remains intact. Very common and often painless
- Herniated disc: The outer layer has a tear, and inner material has pushed through
- Degenerative disc disease: Age-related wear that causes discs to lose height and flexibility
Do I Have a Herniated Disc?
Herniated discs cause specific symptom patterns that differ from muscle strains, with radiating pain that follows nerve pathways being the key distinguishing feature, along with numbness, tingling, or weakness in the leg or arm on one side of the body.
Use this checklist to help determine if your symptoms suggest a herniated disc. Check all that apply:
Radiating pain pattern
- Pain that travels from your back down your buttock and leg (lumbar)
- Pain that travels from your neck down your shoulder and arm (cervical)
- Pain that follows a specific path rather than spreading broadly
Nerve-related symptoms
- Numbness or tingling in your leg, foot, arm, or hand
- Weakness when lifting your foot or gripping objects
- Symptoms worse on one side of your body
Aggravating factors
- Pain worsens when sitting, coughing, or sneezing
- Pain increases when bending forward
- Symptoms change with position (better lying down, worse sitting)
Timing
- Symptoms started suddenly after lifting or twisting
- Symptoms developed gradually over weeks or months
- Pain has persisted longer than two weeks
Quick Self-Check: The Seated Test:
Sit in a chair with your back straight. Slowly extend one leg out in front of you. If this reproduces or worsens your back and leg pain, it may suggest nerve involvement from a disc problem. This is not a diagnosis, but it can help you describe your symptoms to a healthcare provider.
If you checked multiple items in the radiating pain and nerve-related sections, a herniated disc is possible. However, similar symptoms can come from other conditions like piriformis syndrome, spinal stenosis, or muscle problems. Only a healthcare provider can give you a proper diagnosis.
Herniated Disc Symptoms Explained
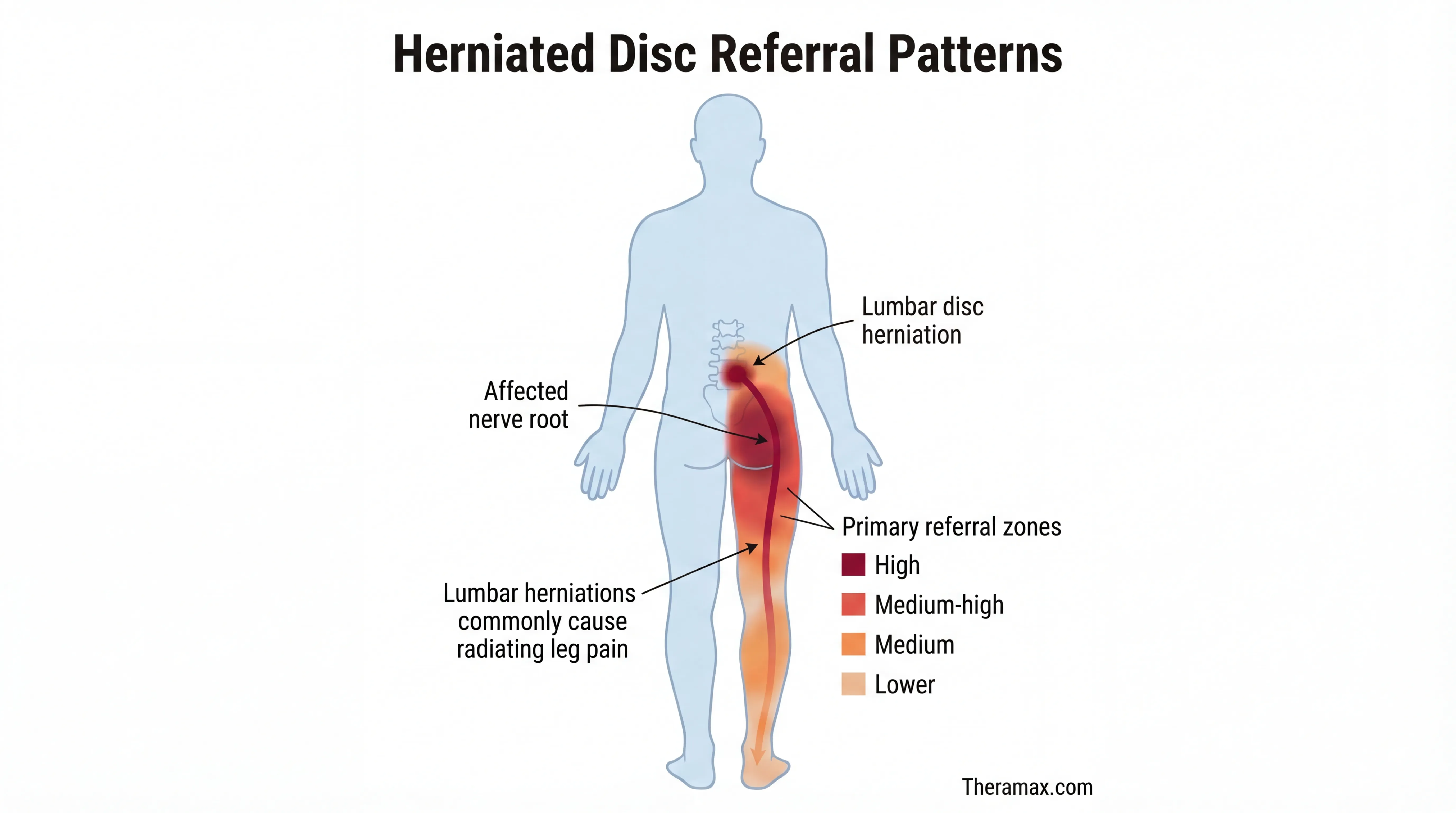
Herniated disc symptoms vary based on the location of the affected disc, with lumbar herniations in the lower back causing leg symptoms like sciatica and cervical herniations in the neck affecting the arms and hands, following predictable nerve pathways.
Lumbar (lower back) herniation symptoms
This is the most common type. Symptoms typically include:
- Low back pain: Often sharp or burning, located on one side
- Sciatica: Shooting pain from the buttock down the back of the leg
- Leg numbness: Often in the calf, foot, or toes
- Weakness: Difficulty lifting the foot (foot drop) or pushing off when walking
- Sitting intolerance: Pain worsens after prolonged sitting, like during long commutes on I-95
Cervical (neck) herniation symptoms
Less common but can be equally disruptive:
- Neck pain: Stiffness and pain at the base of the skull
- Shoulder blade pain: Deep ache between the shoulder blades
- Arm pain: Sharp pain traveling down the arm, often to specific fingers
- Hand symptoms: Numbness, tingling, or weakness in the hand
- Grip problems: Difficulty holding objects or turning keys
Why symptoms appear far from the spine
The nerves leaving your spine travel to distant body parts. When a herniated disc compresses a nerve in your lower back, you might feel it most in your foot. This is called referred pain, and it follows specific nerve pathways. The nerve compressed determines which body part feels the symptoms.
What Causes a Herniated Disc?
Herniated discs develop from a combination of gradual disc degeneration over time and mechanical stress from activities like heavy lifting or prolonged sitting, with certain occupations, genetics, smoking, and excess body weight increasing your risk significantly.
How discs herniate
Discs don't usually herniate from a single event. Most often, the outer layer weakens gradually through years of stress and degeneration. Eventually, a final trigger causes the already-weakened disc to give way.
The four stages of disc herniation:
- Disc degeneration: The disc loses water content and becomes less flexible
- Prolapse: The disc bulges outward but remains contained
- Extrusion: Inner material pushes through the outer layer
- Sequestration: A piece of disc material breaks off entirely

Risk factors
Age: Discs naturally lose water and become less flexible as you age. Most herniations occur between ages 30 and 50.
Occupation: Jobs requiring repetitive lifting, bending, or twisting increase risk. This includes construction workers, nurses, and warehouse employees. Even desk workers in Coral Gables office buildings face elevated risk from prolonged sitting.
Body weight: Extra weight puts additional stress on lower back discs.
Genetics: Some people inherit a predisposition to disc problems.
Smoking: Reduces blood supply to discs, accelerating degeneration.
Sedentary lifestyle: Weak core muscles fail to properly support the spine.
Prevention strategies
- Strengthen your core: Regular exercises that target abdominal and back muscles
- Practice proper lifting: Bend at the knees, keep objects close to your body
- Set up an ergonomic workspace: Monitor at eye level, feet flat on floor
- Take movement breaks: Stand and walk every 30-45 minutes. A quick walk at Coral Gate Park during lunch helps
- Maintain healthy weight: Reduces stress on spinal discs
- Quit smoking: Improves blood flow to spinal structures
Herniated Disc Emergency Signs
Certain herniated disc symptoms require immediate emergency care because they may indicate cauda equina syndrome, a rare but serious condition where a large disc herniation compresses nerves at the base of the spine and can cause permanent damage if not treated within hours.
Go to the emergency room immediately if you experience any of these symptoms:
- Loss of bladder or bowel control (inability to urinate or incontinence)
- Numbness in your groin or inner thighs (saddle anesthesia)
- Severe or rapidly worsening weakness in both legs
- Numbness spreading to both legs
These may indicate cauda equina syndrome, requiring emergency surgery to prevent permanent nerve damage.
Urgent but not emergency situations
See a doctor within 1-2 days if you have:
- Progressive weakness that's getting worse over hours or days
- Fever combined with back pain (possible infection)
- History of cancer with new back pain
- Recent significant trauma (fall, car accident)
When to schedule a regular appointment
See a healthcare provider if:
- Pain persists beyond 2 weeks
- Symptoms interfere with daily activities
- Home care hasn't helped after 2 weeks
- You're unsure what's causing your symptoms
How Herniated Discs Are Diagnosed
Diagnosis of a herniated disc typically involves a physical examination by your doctor to assess nerve function through reflex, strength, and sensation tests, with imaging studies like MRI usually reserved for cases where surgery is being considered or symptoms are not improving.
What happens at your appointment
Your doctor will start with a detailed history of your symptoms: when they started, what makes them worse, and what provides relief. Then they'll perform a physical examination including:
Neurological tests:
- Reflexes: Testing knee and ankle reflexes with a small hammer
- Sensation: Checking if you can feel light touch in different areas
- Strength: Testing muscle power in your legs or arms
- Gait: Watching how you walk
Provocative tests:
- Straight leg raise: Lying flat while the doctor lifts your leg to see if it reproduces symptoms
- Range of motion: Checking how far you can bend, twist, and extend
When imaging is needed
Not everyone with back pain needs an MRI. Guidelines recommend imaging when:
- Symptoms haven't improved after 6 weeks of conservative treatment
- Surgery is being considered
- Red flag symptoms are present (weakness, bladder problems)
- There's concern about other conditions
Types of imaging:
- X-ray: Shows bones but not discs. Useful for ruling out fractures or arthritis
- MRI: Gold standard for seeing disc herniations and nerve compression
- CT scan: Alternative when MRI isn't possible
- CT myelogram: Uses dye to show spinal canal, useful for complex cases
Common MRI Terms Explained:
- Disc protrusion: The disc is bulging but the outer layer is intact
- Disc extrusion: Material has pushed through the outer layer
- Disc sequestration: A piece has broken off completely
- Annular tear: A tear in the outer disc layer
- Foraminal narrowing: The space where nerves exit is smaller
- Central stenosis: The main spinal canal is narrowed
Important: MRI findings don't always match symptoms. Many people have disc abnormalities on MRI with no pain, while some with severe pain have minimal findings. Your symptoms matter more than the scan.
Questions to ask your doctor
- What type of herniation do I have and at what level?
- Which nerve is affected?
- What are ALL my treatment options?
- What is the expected timeline for recovery?
- When would surgery be recommended in my case?
- What can I safely do at home?
- Are there activities I should avoid?
- Should I see a specialist?
- How will we know if treatment is working?
- What happens if conservative treatment doesn't help?
Herniated Disc Treatment Options
Treatment approaches for herniated discs range from rest and home care to physical therapy, spinal injections, and surgery, with 80-90% of patients improving through conservative methods within 6-12 weeks without needing invasive procedures like microdiscectomy or spinal fusion.[2]
The right treatment depends on your symptom severity, how long you've had them, and your overall health. Here's an objective look at all options:
Conservative care (first-line for most cases)
What it is: Rest, activity modification, over-the-counter medications
How it works: Allows inflammation to subside and gives the body time to heal. The disc material may shrink or be reabsorbed over time.
Timeline: 4-6 weeks
Effectiveness: 60-70% of cases resolve with conservative care alone
Pros:
- No intervention required
- Minimal disruption to daily life
- Low risk
- Many cases resolve completely
Cons:
- May not work for severe cases
- Requires patience
- Symptoms may persist during healing period
Best for: Mild to moderate symptoms, recent onset
Physical therapy
What it is: Guided exercise, manual therapy, and education from a licensed therapist
How it works: Strengthens supporting muscles, improves flexibility, and teaches proper body mechanics
Timeline: Typically 6-12 weeks, 2-3 sessions per week initially
Effectiveness: Studies show 70-80% success rate for appropriate candidates[4]

Pros:
- Non-invasive
- Addresses underlying mechanics
- Reduces recurrence risk
- Teaches self-management skills
Cons:
- Requires significant time commitment (multiple sessions over weeks)
- May not work for all cases
- Results depend on patient compliance with home exercises
- Requires referral from some healthcare plans
Availability: Widely available; most clinics offer flexible scheduling
Chiropractic care
What it is: Spinal manipulation and mobilization by a licensed chiropractor
How it works: Aims to restore normal spinal mechanics and reduce nerve irritation
Timeline: Varies; some feel relief quickly, others need ongoing treatment
Effectiveness: Evidence is mixed; many patients report benefit
Pros:
- Non-invasive
- Many patients report pain relief
- No medication required
- Often provides quick symptom relief for some
Cons:
- Evidence base less robust than for physical therapy
- Not appropriate for all herniation types (particularly large extrusions)
- May require ongoing maintenance visits
- Rare but serious risks with cervical manipulation
Availability: Widely available; coverage varies by plan
Spinal injections
What it is: Corticosteroid injection near the affected nerve (epidural steroid injection)
How it works: Reduces inflammation around the nerve, providing pain relief
Timeline: Relief can begin within days; effects typically last weeks to months
Effectiveness: 50-70% of patients experience significant short-term relief[5]
Pros:
- Can provide significant pain relief
- Minimally invasive
- May allow participation in physical therapy more effectively
- Can be diagnostic (confirms nerve as pain source)
Cons:
- Relief is often temporary (weeks to months)
- Does not address underlying disc problem
- Risks include infection, nerve damage (rare)
- Limited number of injections recommended per year
Availability: Requires specialist referral; typically offered by pain management clinics
Surgery
What it is: Surgical removal of herniated disc material pressing on nerve
Common procedures:
- Microdiscectomy: Most common; removes herniated portion through small incision
- Laminectomy: Removes part of vertebral bone to access disc
- Disc replacement: Artificial disc replaces damaged disc
- Spinal fusion: Fuses vertebrae together (for instability cases)
Timeline: Surgery takes 1-2 hours; recovery 6-12 weeks; most resume normal activities in 3-6 months
Effectiveness: 85-95% success rate for appropriate candidates with skilled surgeon[3]
Pros:
- High success rate for appropriate candidates
- Definitive solution for severe cases
- Often provides rapid relief
- May prevent permanent nerve damage
Cons:
- Invasive with surgical risks (infection, bleeding, anesthesia)
- Recovery time required
- Possibility of recurrence at same or other level
- Some patients have persistent symptoms despite surgery
Best for: Failed conservative treatment (6-12 weeks), progressive weakness, cauda equina syndrome, severe unrelenting pain
Herniated Disc Home Care
Effective home care for a herniated disc combines strategic rest with ice and heat therapy, gentle stretches and movement, proper sleep positioning, and over-the-counter medications to manage symptoms while you avoid activities that worsen pain.
Ice vs. heat protocol
First 48-72 hours: Use ice to reduce inflammation
- Apply for 15-20 minutes at a time
- Wait 40 minutes between applications
- Never apply directly to skin (use a towel)
After 72 hours: Heat can help relax muscles and increase blood flow
- Apply for 15-20 minutes at a time
- Heating pads, warm showers, or heat wraps all work
- Never sleep with a heating pad
Some people alternate ice and heat, using ice for acute flare-ups and heat for chronic stiffness.

Safe movements and exercises
Start gentle and stop if pain increases:
- Walking: Often the best exercise. Start with 5-10 minutes, increase gradually
- Knee-to-chest stretch: Lying on your back, pull one knee toward your chest. Hold 30 seconds, 3 times each side
- Pelvic tilts: Lying on your back with knees bent, flatten your lower back against the floor. Hold 5 seconds, repeat 10 times
- Core bracing: Tighten abdominal muscles as if preparing for a punch. Practice maintaining this during daily activities
What to avoid
- Prolonged sitting (more than 30 minutes without a break)
- Heavy lifting
- Twisting movements under load
- High-impact activities (running, jumping)
- Bending forward repeatedly
- Sit-ups and toe touches
Over-the-counter medication guidance
NSAIDs (ibuprofen, naproxen): Reduce inflammation and pain. Take with food. Consult pharmacist about interactions.
Acetaminophen: Pain relief without anti-inflammatory effect. Easier on stomach. Mind daily limits.
Important: Don't exceed recommended doses. If OTC medications aren't helping, see a healthcare provider.
When home care isn't enough
- Symptoms not improving after 2 weeks
- Symptoms getting worse despite rest
- New or spreading numbness or weakness
- Pain interfering with sleep for more than a few nights
Sleeping With a Herniated Disc
Sleep disruption is one of the most frustrating aspects of a herniated disc. Pain often intensifies at night when you're lying still, and finding a comfortable position can feel impossible. The right sleeping setup can significantly reduce night pain and help your body heal.
Why herniated discs hurt more at night
Several factors contribute to increased night pain. During the day, movement keeps spinal fluid circulating and muscles active. When you lie down, discs rehydrate and slightly expand, which can increase pressure on nerves. Additionally, you lose the distraction of daily activities, making pain feel more intense.
Best sleeping positions
Back sleeping (supine)
This position distributes weight evenly and maintains neutral spine alignment. Place a pillow under your knees to reduce pressure on the lower back. The pillow should be thick enough to create a slight bend in your knees. Some people add a small rolled towel under the curve of their lower back for additional support.
Side sleeping (lateral)
Many people with herniated discs find side sleeping most comfortable. Place a firm pillow between your knees to keep your hips aligned and prevent your top leg from pulling your spine out of alignment. Draw your knees up slightly toward your chest in a loose fetal position. Use a pillow that keeps your head level with your spine, not propped up or sagging down.

Elevated legs position (for acute pain)
When pain is severe, try lying on your back with your lower legs resting on a chair, ottoman, or stack of pillows. Your hips and knees should both be at roughly 90-degree angles. This position takes significant pressure off the lumbar discs and can provide relief during acute flare-ups.
Positions to avoid
Stomach sleeping
This is the worst position for a herniated disc. It forces your spine into extension, increasing pressure on the posterior disc where most herniations occur. It also requires turning your head to one side, straining your neck. If you're a lifelong stomach sleeper, transitioning away from this position is one of the most important changes you can make.
Twisted positions
Avoid any position where your shoulders and hips face different directions. This twisting puts rotational stress on your discs.
Pillow setup matters
- Head pillow: Should keep your neck in line with your spine. Too high or too flat both cause problems
- Knee pillow: A firm pillow or specialized knee pillow works better than a soft one that compresses
- Body pillow: Helpful for side sleepers to maintain position throughout the night
- Lumbar roll: A small rolled towel can support the natural curve of your lower back when back sleeping
Mattress considerations
There's no single "best" mattress for herniated discs. The right firmness depends on your body weight, sleeping position, and personal preference. Generally, medium-firm mattresses work well for most people with back problems. The mattress should support your spine's natural curves without creating pressure points.
If buying a new mattress isn't possible, a mattress topper can help. Memory foam toppers conform to your body shape, while firmer toppers can add support to a too-soft mattress.
Getting in and out of bed safely
How you get into and out of bed matters as much as how you sleep. Use the "log roll" technique:
Getting into bed:
- Sit on the edge of the bed near your pillow
- Lower yourself onto your side while simultaneously bringing your legs up
- Keep your spine straight and move as a unit
- Roll onto your back if that's your sleeping position
Getting out of bed:
- Roll onto your side facing the edge of the bed
- Use your arms to push yourself up while swinging your legs off the bed
- Let your legs drop as you rise to sitting
- Stand up by pushing through your legs, not pulling with your back

Managing night pain
- Timing medications: If you use pain medication, taking a dose 30-60 minutes before bed can help you fall asleep more comfortably
- Heat before bed: A warm shower or heating pad before sleep can relax muscles (remove heating pad before sleeping)
- Gentle stretching: Light knee-to-chest stretches before bed may reduce stiffness
- Position changes: It's normal to need to change positions during the night. Having pillows readily available makes adjustments easier
- Getting up if needed: If pain wakes you and you can't get comfortable within 15-20 minutes, get up briefly. Walk around, apply ice or heat, then try again
The Two-Pillow Minimum:
At minimum, keep two pillows on your bed: one for your head and one for your knees (back sleeping) or between your knees (side sleeping). This simple setup can make a meaningful difference in night pain and morning stiffness.
Herniated Disc Recovery Timeline
Most herniated discs improve significantly within six to twelve weeks with conservative treatment, progressing through an acute phase then gradual return to activity, though full recovery may take three to six months depending on the severity of your herniation.
Week-by-week expectations (conservative treatment)
Weeks 1-2 (Acute phase):
- Pain often at its worst
- Focus on rest, ice, and pain management
- Gentle walking if tolerated
- Avoid positions that worsen symptoms
Weeks 2-4:
- Pain should begin decreasing
- Gradual return to light activities
- Can start gentle stretching
- Physical therapy often begins
Weeks 4-6:
- Noticeable improvement for most people
- More active recovery can begin
- Return to modified work activities
- Strengthening exercises introduced
Weeks 6-12:
- Continued improvement
- Gradual return to normal activities
- Many people resume most activities
- Focus on prevention and maintenance
3-6 months:
- Most cases fully resolved
- Return to full activities including exercise
- Some may need ongoing management

Signs of progress
- Pain centralizing (moving from leg toward back)
- Decreased pain intensity
- Improved range of motion
- Returning to activities without flare-ups, like walking through Zoo Miami with family
- Better sleep
Recovery after surgery
If surgery becomes necessary:
- Immediately: Most patients have significant pain relief
- 2-4 weeks: Light activities resume
- 6 weeks: Many return to desk work
- 3 months: Most normal activities resume
- 6-12 months: Full recovery and return to all activities
Herniated Disc Treatment Costs
Understanding herniated disc treatment costs helps you plan financially and make informed decisions about your care, with expenses varying significantly based on the type of treatment, your insurance coverage, and whether you choose conservative care or surgical intervention.
Conservative treatment costs
Physical therapy: $75-200 per session without insurance, typically requiring 2-3 sessions per week for 6-12 weeks. Most insurance plans cover PT with a copay of $20-50 per visit. Total out-of-pocket with insurance: $240-600 for a typical treatment course.
Chiropractic care: $65-150 per session, with most patients needing 8-20 visits. Some insurance plans cover chiropractic; check your specific policy.
Medications: Over-the-counter NSAIDs cost $10-30 monthly. Prescription muscle relaxants or nerve pain medications may cost $20-150 monthly depending on your pharmacy and insurance.
Injection costs
Epidural steroid injections: $1,000-3,000 per injection without insurance. With insurance, expect $100-500 out-of-pocket per injection. A series of 1-3 injections is typical.
Surgical costs
Microdiscectomy: $15,000-50,000 total facility and surgeon fees. With insurance, out-of-pocket costs typically range from $2,000-6,000 depending on your deductible and out-of-pocket maximum.
Spinal fusion: $50,000-150,000 for complex cases. Insurance coverage varies significantly; expect higher out-of-pocket costs.
Insurance considerations
- Pre-authorization: Many insurers require pre-authorization for MRIs, injections, and surgery
- In-network providers: Using in-network providers can reduce costs by 30-60%
- Deductibles: If you haven't met your annual deductible, you'll pay full cost until you do
- Out-of-pocket maximum: Once reached, insurance typically covers 100% of remaining costs
Financial assistance options
- Payment plans: Many providers offer interest-free payment plans
- HSA/FSA: Use pre-tax dollars to pay for treatment
- Hospital financial assistance: Non-profit hospitals often have charity care programs
- Workers' compensation: If your herniated disc is work-related, workers' comp may cover treatment
Cost-Saving Tip:
Starting with conservative treatment like physical therapy is not only medically recommended but also significantly more cost-effective. The total cost of a 12-week PT program is typically less than the out-of-pocket cost for a single epidural injection or a fraction of surgical costs.
Herniated Disc FAQ
Next Steps
Based on what you've learned, your next steps depend on your symptoms. For mild symptoms, try the home care protocol for 1-2 weeks. If symptoms persist, worsen, or include any red flags, see a healthcare provider for evaluation. Bring this guide and the list of questions to your appointment.
For those in Miami exploring physical therapy as a treatment option, TheraMax Physical Therapy provides evaluation and treatment for spine conditions including herniated discs. Our team can help you understand whether PT might be appropriate for your situation.
References
- Herniated lumbar disc. BMJ Clin Evid. 2011 . PubMed
- An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014 ;14 (1) :180-191 . DOI PubMed
- Herniated lumbar intervertebral disk. N Engl J Med. 2016 ;374 (18) :1763-1772 . DOI PubMed
- Surgical versus nonoperative treatment for lumbar disc herniation: eight-year results for the spine patient outcomes research trial. Spine. 2014 ;39 (1) :3-16 . DOI PubMed
- Epidural injections for chronic spinal pain. Pain Physician. 2012 ;15 :E363-E404 . PubMed
- Quality of sleep in patients with chronic low back pain: a case-control study. Eur Spine J. 2008 ;17 (6) :839-844 . DOI PubMed

